Healthcare in America has evolved far beyond the traditional image of a solo practitioner in a small office. Today's healthcare system is a complex network of providers, organizations, and billing entities that can be difficult to navigate—even for industry experts. With the rise of healthcare data analytics and network visualization tools, we can now uncover patterns and insights that were previously invisible. These insights are transforming how healthcare administrators, payers, employers, and policymakers design networks, manage costs, and ensure patients receive the right care.
What are NPIs? Individual vs. Organizational NPIs
At the foundation of healthcare networks are National Provider Identifiers (NPIs), the unique IDs used in claims and billing. Understanding Type 1 vs. Type 2 NPIs is essential:
- Type 1 NPIs identify individual providers such as physicians, nurse practitioners, and therapists.
- Type 2 NPIs identify organizations such as hospitals, group practices, and nursing homes, which often bill on behalf of many clinicians.
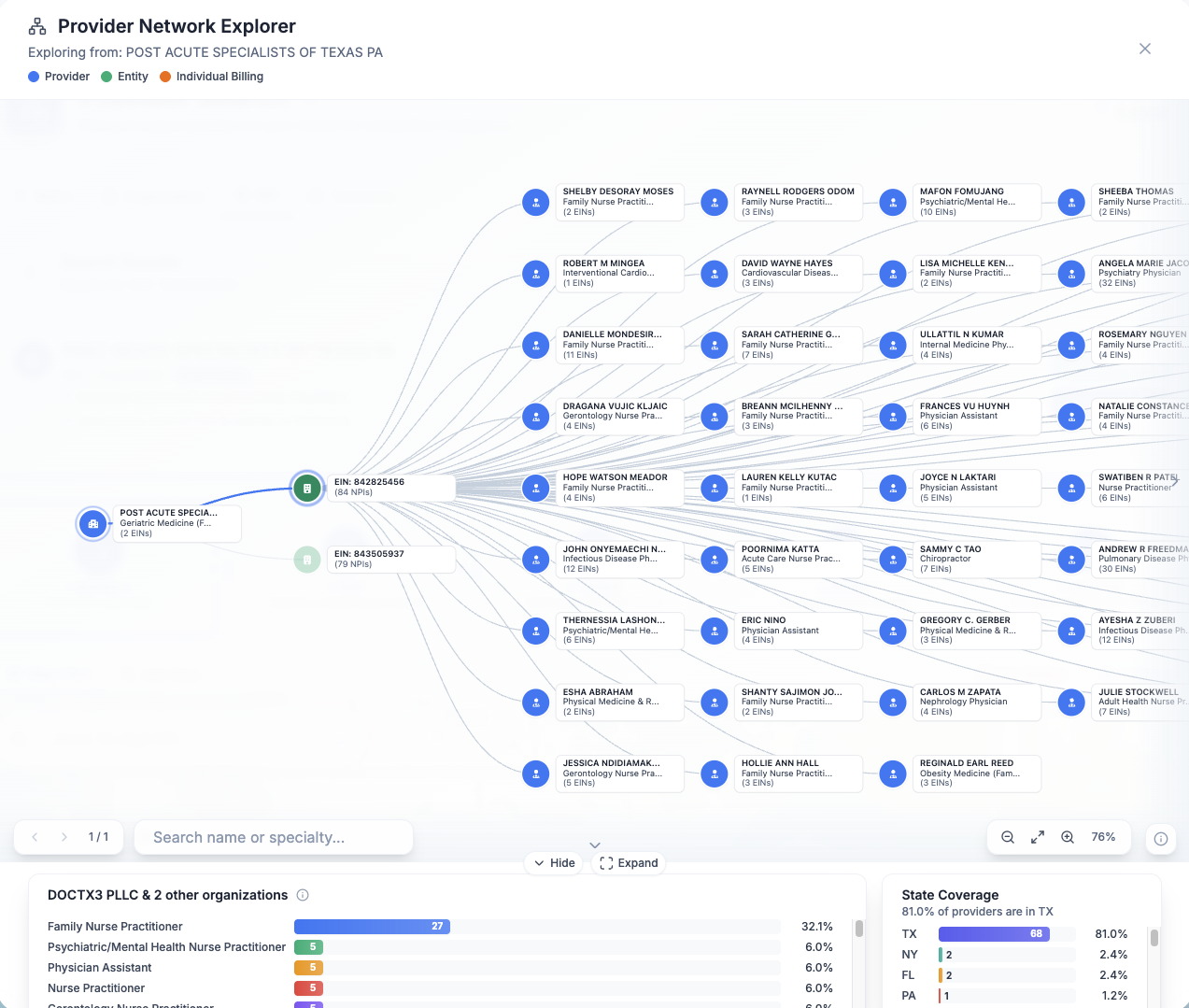
Using federally mandated price transparency data, you can retrieve the EINs (Employer Identification Number) of every organization or billing entity; this allows you to see the full employment structure of provider networks. This creates an extremely powerful tool for benchmarking competitors, making hiring decisions, and targeting markets where there's an opportunity for new health services.
Keeper Health - Provider Network Explorer
One of the most significant trends in healthcare is provider consolidation. Solo practitioners and small groups are increasingly absorbed into larger enterprise health systems and multi-specialty groups.
Keeper Health has the best tool for seeing healthcare billing relationships by binding NPI and EIN and pulling the fee schedules of every provider in the nation. You can identify:
- An EIN with 40% primary care, 30% specialty, 30% behavioral health = integrated, population health model.
- An EIN with 100% orthopedics and PTs = musculoskeletal center of excellence.
- An NPI working with 10 different groups
- An NPI working only as an independent practice.
These insights help payers design networks, providers evaluate opportunities for growth and contract negotiation, and patients understand provider focus.
Practical Applications for Healthcare Leaders
The ability to decode provider networks has real-world value:
For Payers
- Build cost-efficient, adequate networks
- Identify coverage gaps by geography or specialty
- Track consolidation trends impacting contract leverage
For Healthcare Administrators
- Benchmark organizational structure
- Spot merger, acquisition, and partnership opportunities
- Optimize billing and credentialing workflows
For Policymakers
- Monitor market concentration and access in underserved areas
- Evaluate impact of regulations on care delivery
For Employers
- Assess health plan adequacy
- Explore direct contracting opportunities
- Ensure employees have diverse provider access
Why Healthcare Network Analysis Matters
The complexity of modern healthcare networks mirrors the evolution of medicine itself—from solo practitioners to integrated systems capable of delivering coordinated, data-driven care.
By leveraging provider network analytics, NPI mapping, and visualization tools, healthcare leaders can uncover hidden patterns, improve decision-making, and ensure patients access the right care at the right time.
Want to analyze provider networks? Our advanced healthcare analytics platform provides interactive visualizations and actionable insights to help you understand, benchmark, and optimize your provider network relationships.